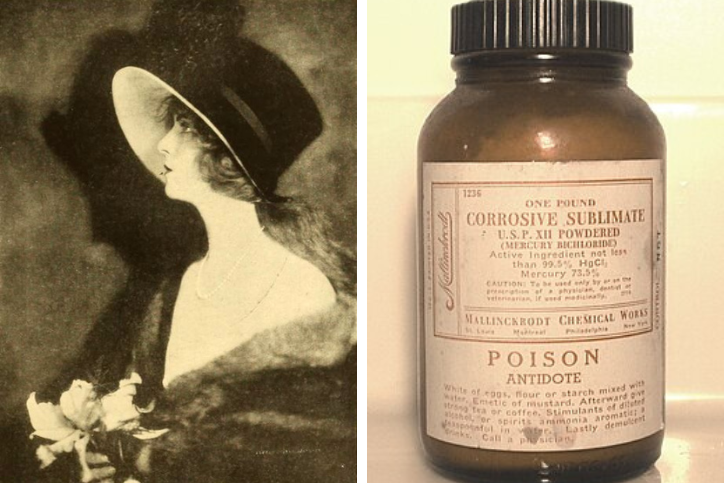
Olive Thomas was a well-known model and silent-film actress in the early 1900s. She died from what was likely accidental poisoning, though there was some controversy about the cause of death at the time.
Olive was traveling on a second honeymoon with her husband to Paris in 1920. Late at night, she drank a solution from the hotel bathroom counter that she likely believed was something to help her sleep. She may have had trouble reading the product’s labeling, as it was late at night so the lighting may have been poor, and it may have been labelled in French, but she was a native English speaker.
Some people wonder if she may have been drinking alcohol or exhausted at the time of the event. All of these are risk factors for accidental poisonings.
What Substance did Olive Actually Take?
It was later found that the solution she ingested was a topical preparation (medicine for the skin) prescribed for her husband. The solution contained a chemical called mercury bichloride that was mixed in alcohol. In the past, mercury was used in disinfectants, antiseptics, and as a treatment for syphilis (a bacterial infection usually spread by sexual contact) before penicillin was invented.
What Medical Treatment was Olive Given?
Her husband and doctors likely attempted many antidotes (something given to prevent a poison from fully acting in the body), such as having her drink excessive amounts of water to induce vomiting or eating egg whites.
Medicine bottles from around this time sometimes listed antidotes such as ingesting:
- egg whites (not the yolk)
- flour or starch mixed with water
- mustard
- strong teas or coffees
- stimulants
The medical profession has since found these, and many other antidotes, to not be effective and we do not recommend them.
Stomach pumping was also a commonly used treatment in this time period. Stomach pumping is similar to a treatment we have today called gastric lavage. This is when a health care provider puts a tube into a patient’s stomach and adds fluid to flush out the contents of the stomach. Both gastric lavage and charcoal are used to decrease the effects of substance on the body. The issue is that charcoal doesn’t work for everything, so the other choice is lavage to flush it out of the stomach.
How Long Did Olive Live After the Poisoning?
Olive lived for five days after drinking the poison. She passed away on September 10, 1920, at 25 years old.
What Does Mercury Bichloride Do to the Body?
The chemical, mercury bichloride, is toxic because it is corrosive and has effects on the kidneys. The corrosion will cause burns to the mouth, throat, and stomach if ingested. This will also cause nausea and vomiting, and sometimes the vomit will contain blood. When the stomach and gastrointestinal tract are injured from corrosion, the body can lose fluid, which can cause blood pressure to drop.
It was believed that Olive called out in pain shortly after drinking the solution, and that later her vocal cords were so badly damaged she could not speak due to the corrosion in her throat.
Ingesting mercury can lead to kidney damage. Acute nephritis (inflammation of kidneys) was mentioned in her autopsy reports as a cause of death.
Was This a Common Cause of Death During Olive’s Time?
Yes, ingesting mercury bichloride was frequently seen as both an accidental and intentional/suicidal ingestion during the 1900s. Other famous cases include Richard Tilghman, who died after taking mercury bichloride tablets thinking they were his lithium medicine, and Madge Oberholtzer, who died by suicide after ingesting the mercury bichloride intentionally.
How Could We Have Treated Olive Today?
Unfortunately, Olive’s mistake was a serious one. Even with today’s advancements in medicine and toxicology, her case would have been difficult to treat. Some of the treatment options that would have been considered include:
- intravenous (administered into a vein) fluids
- medicines to increase blood pressure
- interventions by a gastroenterologist (a doctor that specializes in damage to the gastrointestinal tract)
- being given a chelator (substance that bonds to a metal to remove it from the body) such as giving British Anti Lewisite for mercury
Are People at Risk for Mercury Toxicity Today?
Mercury is a far less significant problem today than it was a century ago. It is no longer used in medicines in the United States.
The most common form of mercury that people are exposed to is methylmercury found inside the fish and seafood we eat. Mercury from the air and other sources settles into stream beds and is converted into methylmercury by the organisms living in the stream. As fish encounter methylmercury in their environment, it is incorporated into their tissue. Nearly everyone who eats seafood has some level of methylmercury within them. However, it is rare for methylmercury levels to be high enough to injure a person. Still there are certain circumstances where methylmercury should be monitored, notably in people who are pregnant and lactating. There is additional information about mercury fish in our previously published fish blog.
Other sources of mercury in the home include:
- old fever thermometers
- certain kinds of novelty jewelry pendants (historically from Mexico)
- antique barometers (instruments used to measure atmospheric pressure)
- skin lightening products (read more about these in our previously published blog about skin lightening products)
- Chinese herbal medications
- light bulbs
What Should I do if I Break a Light Bulb or Fever Thermometer?
If you break a light bulb or fever thermometer, call your local Poison Center at 1-800-222-1222 and they can walk you through clean up. You can also visit the Environmental Protection Agency (EPA)’s website for a list of instructions.
What Can We Learn From This Tragedy?
This is a case where taking the time to confirm the product and the contents of its label would have been extremely helpful. Olive ingested this solution, likely thinking it was another medication. She likely could not or did not take the time to clarify what the bottle contained from the label. We see this simple mistake happen frequently at the poison center even today.
Often times it’s bleach drank by mistake when left in an unlabeled beverage cup or container. Or a tired person grabs the wrong bottle of medication from a crowded shelf and takes the medicine, not checking what it is.
We frequently see poisonings increase when people are traveling, as Olive was. It is easier to make a mistake when in unfamiliar circumstances, such as organizing and storing your medicines differently than you do at home.
Always take time to review what it is you are taking before you take it – your health depends on it! Turn on the light and put on glasses before you try to read a product label.
If you use a household cleaner incorrectly, take a medicine you weren’t supposed to, or need any other poison-related help, do not hesitate to call your local Poison Center for assistance at 1-800-222-1222. It is free to call and poison specialists are available 24/7/365.
Amber Ferrell, PharmD
Certified Specialist in Poison Information



Leave a Reply